Fear of reprisals, 'challenging' reporting process see less than a quarter of abused healthcare workers coming forward
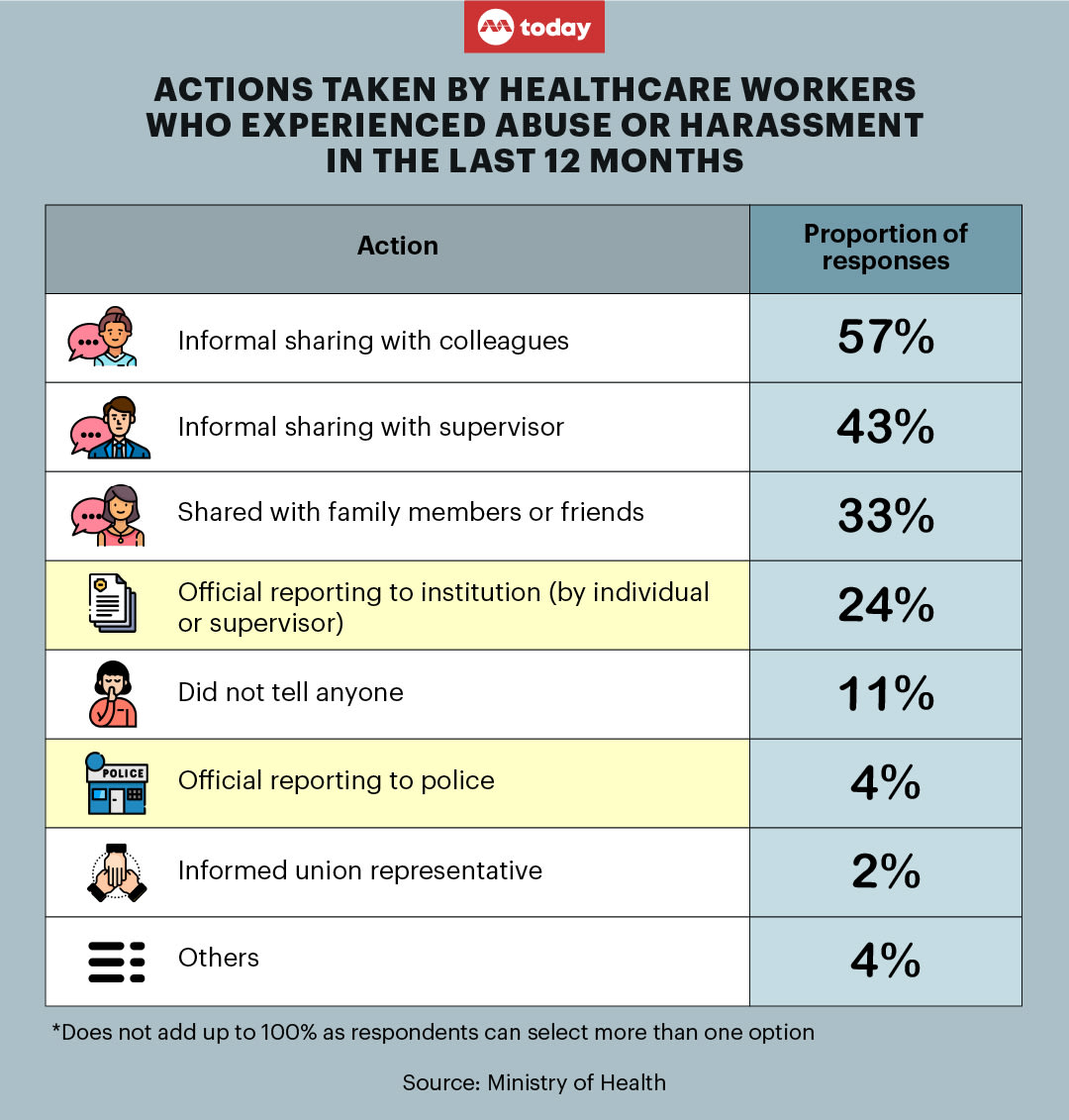
SINGAPORE — Rather than make an official report, a majority of healthcare workers who suffer abuse or harassment at work would casually bring up the incident with their colleagues, while around two in five would do so with their supervisor on an informal basis.

- When faced with workplace abuse or harassment, more healthcare workers would choose to speak about it with their colleagues or supervisor on an informal basis
- A minority of workers who were subjected to abuse or harassment would go on to make an official report
- These were the findings of a study conducted by the Tripartite Workgroup for the Prevention of Abuse and Harassment of Healthcare Workers
- The study also found that shortcomings in the reporting process and negative perceptions within the industry around reporting such incidents deterred healthcare workers from coming forward
- The Health Ministry will work with public healthcare clusters from the second half of 2023 to develop a zero-tolerance approach
SINGAPORE — Rather than make an official report, a majority of healthcare workers who suffer abuse or harassment at work would casually bring up the incident with their colleagues, while around two in five would do so with their supervisor on an informal basis.
And despite the existence of processes by all healthcare institutions for reporting and investigating such abuses, fewer than a quarter, or 24 per cent, of healthcare workers who experienced such situations in the past year reported it to their institutions, a study by a tripartite workgroup found.
The findings of the study by the Tripartite Workgroup for the Prevention of Abuse and Harassment of Healthcare Workers, which was published in a Ministry of Health (MOH) press release on Friday (March 17), were derived from surveys and focus group discussions with more than 3,000 healthcare workers and more than 1,500 members of the public over the course of a year.
The workgroup is established by MOH and comprises ministry representatives, as well as those from the Healthcare Services Employees’ Union, public healthcare clusters, community care partners and private healthcare providers. It was formed in April 2022 in light of rising rates of abuse and harassment of healthcare staff members.
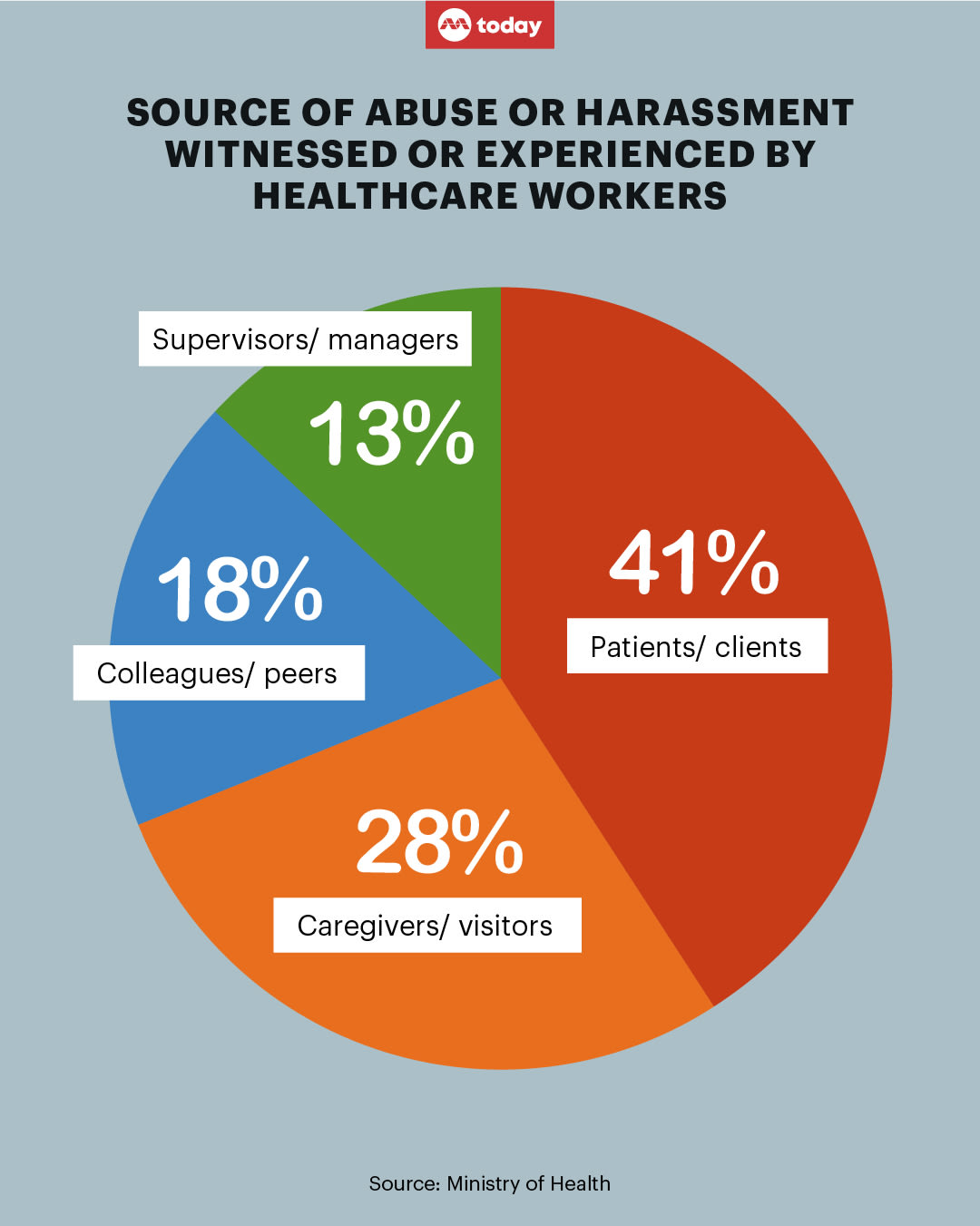
Its report also found that more than two in three healthcare workers had witnessed or personally experienced abuse and harassment in the past year.
In spite of this, the lack of clarity regarding what constituted abuse, coupled with shortcomings in the reporting process as well as negative perceptions within the industry around reporting such incidents, deterred healthcare workers from making reports.
As such, a survey of healthcare workers who experienced abuse or harassment in the last 12 months found that 57 per cent of respondents would talk about it informally with their colleagues, and 43 per cent would do so with their supervisors.
Only 4 per cent made a police report, while around 11 per cent of the healthcare workers polled kept the incidents to themselves.
Speaking at an engagement session with healthcare workers from the National Healthcare Group at the Ng Teng Fong Centre for Healthcare Innovation on Friday, Health Minister Ong Ye Kung said: "When an incident of abuse has been escalated and ascertained, the staff must feel that he is not alone, and people around him are behind him — his supervisor, management, the ministry, the minister, and most importantly, the great majority of the public."
"It cannot be the case where a supervisor takes action to disengage from an abuser, the abuser complains to the Member of Parliament or the Minister for Health, and the supervisor gets reprimanded for bad service. We will have to stand together on this, against the very small minority of abusers," he added.
SHORTCOMINGS IN REPORTING ABUSE
The survey found that as part of the process of escalating a case, the abused healthcare workers were sometimes made to recount the incident repeatedly to different supervisors and managers, which could be challenging especially if they were emotionally affected.
The reporting process was also cumbersome, often requiring healthcare workers to file reports outside of their working hours. If processes such as interviews at the police station took place during working hours, healthcare staff would need to take time off from work.
Additionally, they were concerned about how reporting such incidents would be perceived by their supervisors and colleagues, and feared they would be seen as over-reacting. Foreign healthcare workers, in particular, were worried that they would lose their jobs.
In instances where cases of abuse and harassment were reported, some of the abused healthcare workers surveyed by the workgroup felt there were limits to action that could be taken against offenders, and also preferred if more timely updates on the outcome of their reports could be given.
ZERO-TOLERANCE APPROACH
The report then recommended a standardised zero-tolerance policy against abuse and harassment to be implemented across all healthcare institutions.
This could include refusing unreasonable requests in cases where the patient does not require urgent medical care. Abusive patients may also be discharged.
The workgroup proposed that abuse and harassment be commonly defined as “any threatening, abusive or insulting words, behaviour or communication that may cause a healthcare worker to experience distress, harassment, threat or discrimination, even if the individual did not intend to do so”.
This means that abuse and harassment by patients or their caregivers include the following:
- Repeated incidents or behaviour that may have a cumulative impact on healthcare workers’ emotional or psychological well-being
- Abuse and harassment that has taken place regardless of the intention of the perpetrator, including by those with cognitive impairment, who are confused, or with dementia
- Online "doxxing", or the publication of the identity of the healthcare worker
- Threats that may include reputational, financial or physical harm
- Any discrimination due to race, religion, gender, nationality or language
Apart from establishing a standardised definition, the workgroup also recommended that the reporting and escalation protocol be strengthened to boost healthcare workers’ confidence and assurance.
This includes follow-ups on each report with independent investigation and transparent feedback on its outcome, whether from the institution or the police where relevant, the report stated.
In the event of abuse or harassment, institutions should ensure there is a clear internal protocol or line of action, which could include issuing a warning to the perpetrator or disengaging by refusing unreasonable requests.
“Staff should have basic knowledge on how to identify and handle abuse and harassment, and be ready to call out such behaviour when they or their colleagues encounter it,” said MOH in its press release.
They should also be trained in effective communication and de-escalating tense situations with patients, as well as educated on the appropriate response to adopt in high-risk situations, MOH added.
WHAT WILL BE DONE
From the second half of 2023, MOH said it will work with public healthcare clusters to develop this zero-tolerance policy, which will be led by public health institutions.
“Private healthcare institutions and community care organisations will be encouraged to refer to the parameters of this zero-tolerance policy when designing or updating their internal processes,” said MOH.
In addition, the tripartite group will work with MOH to implement a national public education campaign promoting mutual respect and positive relationships between healthcare workers and their patients and caregivers. It will be launched in the latter half of this year.
Noting that the tripartite workgroup “takes a firm stand that there should be no tolerance for abuse or harassment of healthcare workers, regardless of the intention and circumstance”, MOH said that a balance should ultimately be struck “to ensure that a positive relationship of trust and respect is maintained between healthcare workers and their patients”.