SGH lapses to blame for hepatitis C outbreak
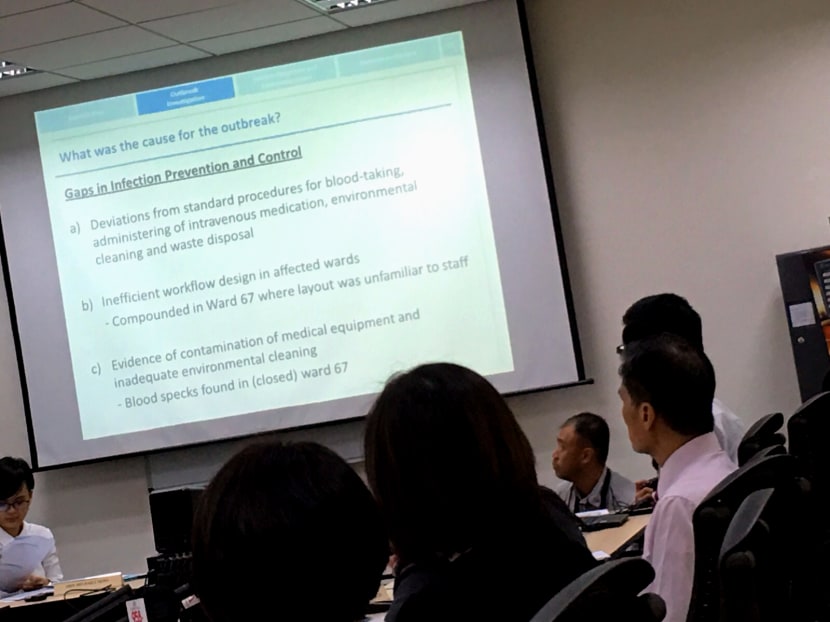
SINGAPORE — The hepatitis C outbreak in Singapore General Hospital (SGH) earlier this year was most likely caused by multiple overlapping factors, with the hospital’s gaps in infection prevention and control measures part of these, an independent review committee that investigated the episode has found.
The independent review committee held a media briefing and released its report on the SGH hepatitis C outbreak to the media on Dec 8, 2015. Photo: Raymond Tham
SINGAPORE — The hepatitis C outbreak in Singapore General Hospital (SGH) earlier this year was most likely caused by multiple overlapping factors, with the hospital’s gaps in infection prevention and control measures part of these, an independent review committee that investigated the episode has found.
SGH also failed to recognise the outbreak in two of its wards in a timely way, said the committee led by infectious diseases expert Leo Yee Sin in its report released today (Dec 8).
The outbreak between April and August this year affected 25 patients, of whom eight have died — seven with hepatitis C likely contributing to their deaths. The contributory causes noted by the committee included the fact that the affected wards housed kidney transplant patients whose immune systems were compromised.
All affected patients were exposed to intravenous medication and had their blood taken, which exacerbated the risk of hepatitis C spreading through gaps in infection control.
The move from Ward 64A to 67 in April — for renovations — was also a factor, as the layout was different from what hospital staff were familiar with, added the seven-member committee, which was appointed on Sept 28 and had access to other resource persons and international experts.
Its 81-page report was submitted to Health Minister Gan Kim Yong last Saturday. The Ministry of Health (MOH) and SGH have accepted the committee’s findings.
The committee also said Singapore’s current system works well for community outbreaks and healthcare associated infections, but is not able to detect unusual infections such as Hepatitis C, which is not easily picked up by surveillance due to a relatively long and variable incubation period, and patients not showing symptoms.
SGH had stepped up infection control measures from early June and this helped to slow the spread of infection, said the committee. But gaps were still found when site visits were done months after the outbreak, in October and November.
For instance, blood stains were found on computerised medical carts, procedure trolleys and on the wall of the preparation room that was supposed to be “clean”. In fact, the stain on the wall of Ward 67’s preparation room tested positive for Hepatitis C genetic material — although this did not mean the virus was still alive and infectious, noted Prof Leo.
Cleanliness and infection control for the affected group of patients cannot be overemphasised, said Professor Lim Seng Gee, a committee member. Extremely high quantities of the virus were found in affected patients, with one drop of blood containing at least 5 million viruses, he said.
Multi-dose vials, which were pinpointed for blame early on when news of the outbreak surfaced, cannot fully explain the virus transmission among the patients, as only 13 of the 25 affected were exposed to them.
By mid-May, SGH’s renal unit was suspicious of an initial cluster of four Hepatitis C cases but had thought this was possibly due to the switch to a more sensitive test for the virus in 2014.
SGH began its own investigations into the cluster in mid-May but they were incomplete, with more elements looked into after a meeting on Sept 3 with the MOH’s Director of Medical Services, Associate Professor Benjamin Ong. It did not escalate the matter to MOH until it felt its own investigations were completed.
SGH also did not escalate the matter to its parent SingHealth and SingHealth’s group chief executive was only informed on Sept 3.
Earlier escalation from the hospital to SingHealth or to MOH could have meant additional resources and expertise to manage the outbreak, the committee said. But Prof Leo said it is difficult to speculate if fewer people would have been affected.
Despite the gaps in identifying, managing and reporting the outbreak, the committee found no evidence to suggest deliberate delay in escalating the matter to the Director of Medical Services.
Assoc Prof Ong, who asked SGH at the Sept 3 meeting for more investigations into the severity and extent of the outbreak within two weeks, had also done the “professionally valid and appropriate” thing, said the committee. Mr Gan was informed on Sept 18 and briefed by SGH on Sept 25.
The committee would not say what would have been a timely period for SGH to inform Assoc Prof Ong of the outbreak.
“It’s always easy, in retrospect, to say, ‘They should’ve done this at this time’,” said Prof Lim. But it is not easy for clinicians to make the call in the heat of handling Hepatitis C diagnoses and jaundice cases, he said. “The second issue is that the ministry really didn’t have a strategy to deal with this type of outbreak, so it was a two-fold problem.”
Professor Tan Chorh Chuan, a resource person of the committee, added that it is important for hospitals to take ownership of the issue and develop expertise to manage such outbreaks. If they lack the expertise, they should be able to have a dialogue with the ministry early on to make sense of the situation and gain access to more resources. But “it is also important to avoid a situation where hospitals say that their job is just to inform the ministry and then the ministry has to then do everything else”, he said.
Both Mr Gan and SGH chief executive Ang Chong Lye apologised to affected patients and their families today, with Mr Gan calling it a painful incident for “all of us” and pledging to learn and improve from the episode. Both ministry and the hospital announced the setting up of human resource panels to examine the responsibilities and actions of key staff involved in the outbreak, and to assess if disciplinary action should be taken.
The ministry will also set up a taskforce led by Minister of State for Health Chee Hong Tat, to enhance the Singapore healthcare system’s ability to detect and respond to infectious disease outbreaks in hospitals and the community.
Asked why a Committee of Inquiry was not convened for the outbreak, Mr Gan told reporters at a doorstop interview that doing so would be to repeat the work that the independent review committee has done, which he is satisfied was comprehensive and has adequately covered all the key areas.
He added: “The priority now is really to focus on implementing the recommendations so that we can continue to improve patient care and patient safety.”









