Skin problems from frequent washing, sanitising of hands ‘unavoidable reality’ during Covid-19
SINGAPORE — In the last few months, senior patient service associate Judy Tan, 56, who works at the National Skin Centre, has been struggling to find a balance between managing her eczema-prone skin and maintaining tip-top hand hygiene at work.
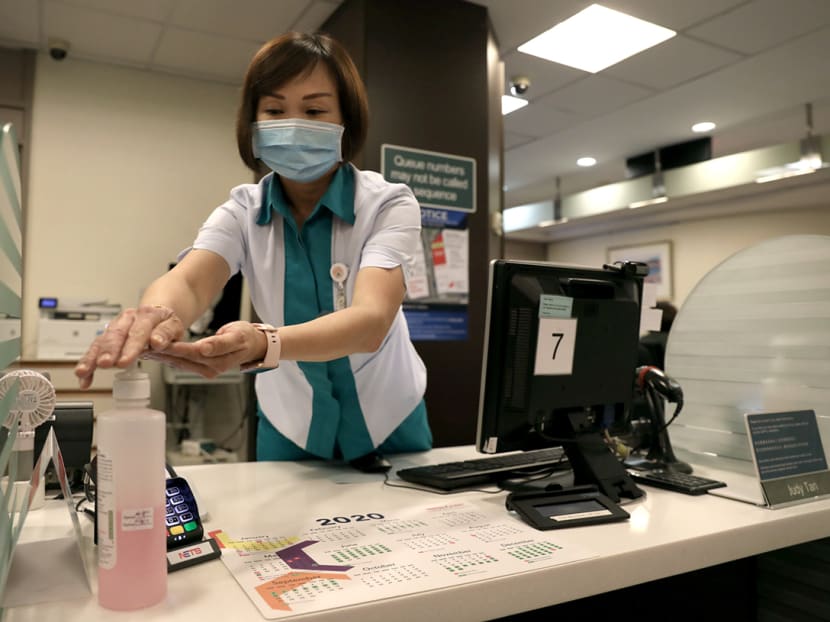
Senior patient service associate Judy Tan (pictured), who works at the National Skin Centre, said that she and the majority of her colleagues are having dry, itchy hands from the vigorous hand washing and sanitising needed on their job.
SINGAPORE — In the last few months, senior patient service associate Judy Tan, 56, who works at the National Skin Centre, has been struggling to find a balance between managing her eczema-prone skin and maintaining tip-top hand hygiene at work.
Ms Tan suffers from irritant hand eczema on her right hand, a skin disease commonly seen in people working in the healthcare and food industry due to stringent hand hygiene practices.
Her work at the National Skin Centre involves handling patient enquiries, clinic registration as well as appointments and billing matters.
The eczema on her hands, which started about two years ago, has left her with painful, dry and cracked skin. Sometimes, the cracked skin would bleed.
Even the simple act of washing the dishes or shampooing her hair is challenging when her skin acts up.
The ongoing Covid-19 pandemic has made it even more challenging for her as healthcare workers must sanitise their hands after each patient encounter.
Ms Tan, who works in a subsidised dermatology clinic where she sees up to 100 patients each day, said: “I try to wash my hands with soap and water, and then apply moisturiser after handwashing in between patients instead of using alcohol rubs, which really hurt my skin.
“If I have to use alcohol rubs or disinfectant wipes to clean the table counters at work, I will use the other hand, which is still holding up at the moment.”
Ms Tan said that her skin issues are not unique. Since the authorities stepped up on infection control measures, many of her colleagues have also been experiencing similar symptoms.
That is why the National Skin Centre is now appealing to companies for donations of hand moisturisers such as lotions and creams to support its affected healthcare workers during this crisis. Companies who wish to do so may get in touch with the centre via email at pr [at] nsc.com.sg.

Ms Tan said: “Like me, the majority of my colleagues are also experiencing dry, itchy hands. However, I am honoured and proud to be in healthcare at this critical moment, so I will still carry on and do my part even though my hand eczema affects my lifestyle.”
She has sought treatment at the skin centre itself. For now, she uses olive oil and hand cream, and wears cotton gloves at night after applying moisturisers to ease her severe skin dryness.
SANITISING HANDS 30 TO 50 TIMES EACH WORK SHIFT
Good hand hygiene helps prevent the transmission of infections such as Covid-19, but these preventive practices can also damage the skin.
Anecdotally, dermatologists approached by TODAY said that they are seeing a rising number of people with irritant eczema in the last two months — all related to increased handwashing and overuse of harsh sanitising and disinfecting products.
Dr Mark Tang, senior consultant dermatologist at The Skin Specialists and Laser Clinic, said that skin issues related to over-washing and hand hygiene practices are an “unavoidable reality” for many people at the moment, particularly for healthcare and frontline workers.
He said that medical personnel must sanitise their hands after every patient encounter, which could be 30 to 50 times for each shift.
“Being a little obsessive about hand hygiene is important and even life-saving at this time.
“For those with a predisposition for hand or facial eczema, it is a very difficult time for them to balance the dilemma of maintaining hand hygiene and preventing eczema flares,” Dr Tang said.
RASHES ON FACE FROM WEARING MASKS
Dr Tang has also encountered cases of facial rashes and mild pressure sores due to prolonged wearing of surgical or face masks.
The skin doctor, whose clinic is in Mount Alvernia Medical Centre, sees around two to three cases of hand rashes and one to two cases of facial rashes a week.
This does not include the many “informal consultations” he has when he encounters other healthcare workers in the wards and along corridors.
Dr Suzanne Cheng, senior consultant at the National Skin Centre, said that she has also noticed an increase in irritant eczema on the arms, legs and trunks due to frequent use of antiseptic body washes.
In particular, those with pre-existing eczema will suffer more because they already have a defective skin barrier, which makes their skin more sensitive.
DISRUPTING THE SKIN’S NATURAL BARRIER FUNCTION
Dr Cheng said that handwashing with soap and other aggressive disinfectants strip the skin of natural oils and damages the skin barrier.
When this is repeatedly done, it can cause skin dryness and flaking. In more severe cases, there is skin inflammation, itch, cracks and soreness.
Frequent use of an alcohol-based hand rub as well as disinfectant wipes and solutions for decontamination of high-touch areas has a similar effect, she added.

Even for those without pre-existing eczema issues, dermatologist Lynn Chiam from Children and Adults Skin Hair Laser Clinic said that certain ingredients found in hand sanitisers and detergents can disrupt the natural barrier function of the skin and strip away the skin’s natural oils and reduce its ability to protect itself.
The ingredients used in hand sanitisers that may affect the skin include various forms of alcohol, such as ethanol, n-proponol, isopropyl alcohol, chlorehexidine, hydrogen peroxides, quaternary ammonium derviatives, colorants and fragrances, Dr Chiam said.
So, although dermatologists see irritant eczema more commonly in people working in the healthcare and food sectors who must wash their hands more frequently, Dr Cheng from the National Skin Centre said that “almost everyone” now can develop the skin disease due to more vigorous hand hygiene practices to limit transmission of Covid-19.
Dr Chiam said that besides the healthcare sector, those working in the education and childcare sectors are more likely to sanitise and wash their hands more frequently as well.
In her practice, she has seen a 20 per cent increase in patients with hand eczema in the last two months. They range from young adults to parents of young children to the middle-aged group.
“In severe cases, both hands are cracked, fissured and bleeding. It is painful (for them) to open their hands as the skin is so dry and painful,” she said.
One of Dr Tang’s patients, a 34-year-old auditor who did not want to be named, said that excessive handwashing in the last few months following the birth of her first child have worsened her hand eczema.
Right now, the dry and irritated skin around her joints has started to split spontaneously, which causes her a lot of pain.
“I wash my hands even more these days, especially after I touch lift buttons or door handles. When well-meaning colleagues offer me hand sanitisers, I’ll feel obliged to use them even though the alcohol rubs burn my skin so much that I feel like screaming when I use them,” she said.
Dr Tang said that some of the more severe cases he has seen have infected areas with crusting and oozing. Tiny water vesicles (fluid-filled blisters) as well as swollen and inflamed nail folds can also develop.
“These patients have constant itch that can affect their sleep. They also scratch incessantly, leading to further worsening of the inflammation and infection,” he said.
CRACKED SKIN RAISES RISK OF ACQUIRING INFECTIONS
While good hand hygiene helps prevent transmission of infections, the experts warned that skin that is cracked and damaged could, ironically, put people at a higher risk of acquiring infections.
Dr Chiam said: “Over-washing and over-disinfecting our hands can lead to excessive stripping away of natural oils on the skin, which are important components of the skin barrier. With a defective barrier function and cracks, tears in the skin from dryness, bacteria and viruses can enter the skin more readily.”
Dr Tang said that although broken and fissured skin may increase the risk of bacterial infections and certain skin viruses such as the human papillomavirus that can cause warts, it does not increase one’s risk of getting respiratory viral infections such as Covid-19 per se.
This is because respiratory viruses are usually transmitted via the respiratory tract or mucosal lining.
However, he pointed out that people with hand rashes may not adhere closely to hand hygiene practices due to their skin condition.
“These lapses can increase their personal risk of getting infected. So, early prevention and treatment of hand rashes are vital in our fight against the pandemic,” Dr Tang said.
A GENTLE CLEANSER WILL WORK JUST AS WELL
For those prone to getting eczema or have active eczema, Dr Cheng of the National Skin Centre advised avoiding or minimising contact with irritants such as soap, disinfectants, detergents and alcohol-based wipes and rubs.
“Use a gentle, soap-free, fragrance-free cleanser instead. Ensure there is easy access by putting a bottle by the sink, shower room and at your workplace toilet.
“A cleanser does not need to be antibacterial or industrial-strength to clean skin and remove dirt, bacteria and viruses,” she emphasised.
She also cautioned against using hot water to wash hands or shower because it can worsen skin conditions. The temperature of the water using for handwashing does not impact the removal of germs such as bacteria or viruses that cause diseases.
Associate Professor Hsu Li Yang, programme leader for infectious diseases and the co-director of global health at NUS Saw Swee Hock School of Public Health, said that regular handwashing works best to clean hands, but added that a hand sanitiser is useful when a tap is not readily available.
“Regular soap is sufficient to pry apart the envelope of viruses such as Sars-CoV-2, which causes Covid-19, while water additionally washes away the virus particles, which does not happen with hand sanitiser,” Associate Prof Hsu said.
He explained that most of the active ingredients in hand sanitisers available will work against the coronavirus, particularly those containing alcohol above 60 per cent concentration.
However, cleansers marketed as “antibacterial” offers no advantage against viruses, he said. They act against bacteria instead.









