What fertility patients should know about egg freezing
NEW YORK — The failure of systems used to store frozen eggs and embryos at two fertility clinics in the United States has rattled people who count on such clinics to help them realise their hopes of having children.
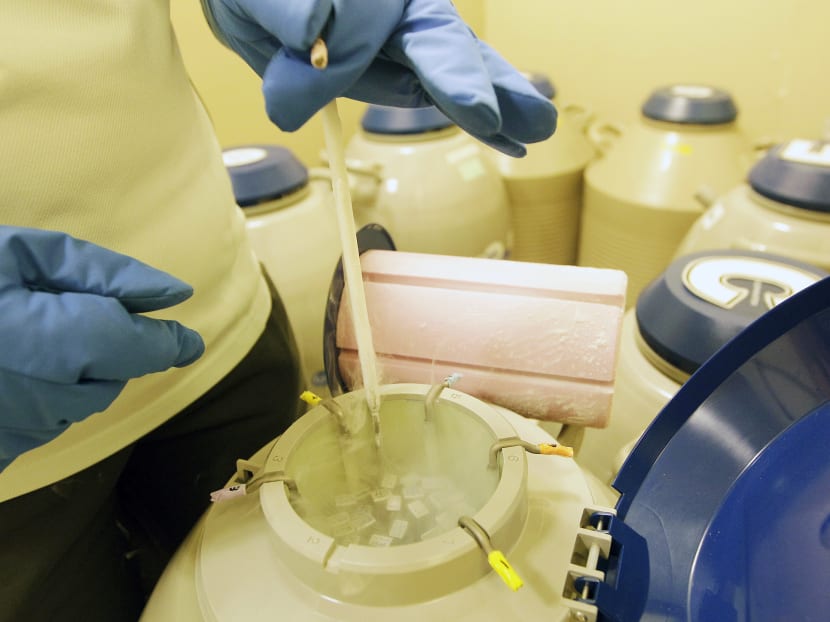
An employee checks oocytes and embryos (in the sealed test tubes) in tanks filled with liquid nitrogen in a storage room at a reproductive centre. While more than 20,000 American women have had their eggs frozen, the vast majority have not had their eggs thawed. Photo: Reuters
NEW YORK — The failure of systems used to store frozen eggs and embryos at two fertility clinics in the United States has rattled people who count on such clinics to help them realise their hopes of having children.
But the breakdowns at clinics in Cleveland and San Francisco, each apparently involving the temperature or level of liquid nitrogen in one storage tank, have damaged at least some eggs and embryos belonging to potentially hundreds of people.
At a time when egg freezing is increasing swiftly — some Silicon Valley companies now tout it as a perk for their employees — the incidents raise questions about what to look for and ask if you are considering taking that step. Here is a basic guide:
HOW LIKELY ARE STORAGE FAILURES?
Several doctors with years of experience in the fertility industry say the recent incidents in San Francisco and Cleveland appear to be unusual.
“I’m not aware of any other instances,” said Dr Catherine Racowsky, the director of the IVF lab at Brigham and Women’s Hospital in Boston, who has served on several professional and government oversight committees.
Dr Racowsky and others said that fertility clinics tend to have backup systems to handle technical failures and make sure frozen tissue stays frozen.
“It’s every clinic’s nightmare,” said Dr Julie Lamb, director of fertility preservation at Pacific NW Fertility in Seattle.
She has been fielding questions this week from concerned patients, assuring them that the clinic has multiple backup storage tanks, freezers checked by staff members twice daily, and a “specialised alarm system that monitors tanks, monitors the temperature in the nitrogen level and is connected to a whole phone system with multiple layers of alarms.”
Mr Jake Anderson, a founder of Fertility IQ, a website that provides assessments of fertility doctors and clinics, noted that both the Cleveland and San Francisco clinics are “large, reputable, subject to oversight,” and they both quickly acknowledged the failures publicly.
But he said he worried about smaller, private clinics that have no affiliation with a university or hospital and whether some would be less inclined to disclose a problem.
“If this happens in other places that are private, people would take this to the grave and they would never breathe a word of this,” Mr Anderson said. “To think that only the well-run places that have boards and clinical oversight — they’re the only ones having this problem? I believe the opposite.”
THE TECHNOLOGY YOU SHOULD ASK FOR
A change in freezing technology in recent years has made things easier. The previous technique, slow freezing, could create ice crystals, which could damage the eggs when they were thawed, said Dr Randi Goldman, a clinical instructor of reproductive endocrinology and infertility at Harvard and Brigham and Women’s Hospital.
Several years ago, clinics began using a process called vitrification, in which the temperature of the eggs in the liquid nitrogen is dropped so quickly that they are frozen “truly in a matter of a second,” Dr Goldman said.
Eggs frozen by that method are less vulnerable to damage when thawed.
“You should ask if a clinic is doing vitrification, but that’s table stakes,” Mr Anderson said. “If someone says they’re not doing vitrification, you should run the other way.”
Clinics that have experience thawing eggs have often worked with donor eggs from young women in their 20s. These eggs may be more likely to thaw without damage, and are undoubtedly more likely to produce healthy pregnancies and babies.
Last year, Dr Goldman and her colleague Janis Fox, published a study based on a mathematical model that attempts to predict a woman’s chances of giving birth to a child from eggs she has frozen.
Their publicly available calculator factors in the woman’s age (the older she is, the lower her chances) and the number of eggs she has frozen (the more the better). Their study estimates an 85 per cent successful thaw rate for women who were 36 and over when they froze their eggs, 95 per cent for women who were under 36.
But thawing without damage does not mean a baby will ultimately be born. After thawing, an egg must be fertilised with sperm in the lab using a process called intracytoplasmic sperm injection or ICSI.
“I think patients may be under the misimpression that we’re just going to put the eggs back in your body,” Dr Fox said.
Far from it. An egg must be fertilised, grown into an embryo for about five days, screened for genetic abnormalities and then implanted in the womb and carried to term. The odds of success at each step are far below 100 per cent.
Dr Fox and Dr Goldman’s calculator, for example, predicts that a 36-year-old woman who freezes 10 eggs has a 60 per cent chance of at least one live birth. A 2016 study by researchers in Spain, which involved 137 women whose frozen eggs were thawed, was less optimistic, predicting that women 36 and older who freeze ten eggs have a 29.7 per cent chance of giving birth.
WHAT ARE SOME OTHER ASPECTS OF EGG FREEZING TO BE AWARE OF?
Since younger eggs are more likely to produce successful pregnancies, women might think they should freeze their eggs in their 20s. Dr Goldman and Dr Fox advise against that.
“Assuming you have normal fertility and nothing unusual in your family history, there’s definitely a point where it’s too early, and we don’t know what the shelf life of these eggs are,” said Dr Fox, who cited a study saying “the most effective age to do it was 34 but the most cost-effective age to do it was 37.”
It’s hard to compare clinics because they may serve different patient populations.
Mr Anderson recommends asking the clinic’s fertilisation rate — “if it’s below 70 percent, it’s a nonstarter,” he said — and it’s “embryo conversion rate,” the percentage of fertilised eggs that become embryos.
“Below 40 per cent you should walk out the door; 40 to 50 per cent - that’s a stay, they’re competent.” Above 50 per cent, he said, is “pretty spectacular.”
It is also worth asking how many embryologists a clinic has, he and others said.
“There should always be at least two embryologists in the lab at all times,” Dr Racowsky said. THE NEW YORK TIMES









