How often you should get a cancer screening and why tumour-marker tests don't always detect cancer
SINGAPORE — In Singapore, an average of 46 people were diagnosed with cancer daily and 16 people died of cancer each day for the period from 2017 to 2021.

Ms Amaliah Othaman (right) at the Singapore Cancer Society Clinic@Bishan.

This audio is AI-generated.
- Cancer screening can help detect early signs of cancer, sometimes even before symptoms appear
- However, not all cancers have well-established, effective screening methods
- For instance, tumour-marker tests may look normal even in someone with advanced cancer
- They are therefore generally not recommended as a form of routine cancer screening
SINGAPORE — In Singapore, an average of 46 people were diagnosed with cancer daily and 16 people died of cancer each day for the period from 2017 to 2021.
One in four people may develop cancer in their lifetime, the Singapore Cancer Society also states on its website.
So screening for cancer is not such an abnormal thing to do.
Do you know, for example, that there is a national screening programme, or that there are screening guidelines for some common cancers such as colorectal, breast and cervical cancers?
And if you want to get started, do you know which tests to take in relation to cancer detection?
For instance, do you really need to check the boxes for all the tumour-marker tests that add to your total bill when you go for a health screening package?
With cancer, early detection and treatment are key to better clinical or management outcomes. TODAY speaks to some doctors to find out what to consider when deciding on screening tests.
As is usual, people generally do not think that they will get cancer, especially if they perceive themselves as being rather healthy.
Take 41-year-old Amaliah Othaman, who is Singaporean and has two children.
She decided in 2019 to get her health checked after finding a lump in her breast and it turned out to be benign.
“From there, I thought that maybe I should just check out what screenings are available and go for them,” she said.
She came upon a free Pap smear or a Pap test offered by the Singapore Cancer Society.
In her mid-30s at the time, she had never gone for a Pap test that involves collecting cells from the cervix, which is located at the lower part of the womb.
Women who are 25 years old and above and have ever had sex are recommended to go for cervical cancer screening.
The test saved her life. The results came back to show that she had Stage 1 cervical cancer.
Recalling her shock upon learning of the diagnosis, she said: “I remembered wondering, ‘How is it possible?’ I felt perfectly fine – I had no symptoms, was living an active life and seldom fell sick."
The cancer diagnosis was a big wake-up call to take her health screenings seriously, she added.
Having gone for treatments and survived cancer for almost five years, Ms Amaliah now encourages her family and friends to get screened regularly for peace of mind.
“The doctor told me that I was very lucky to detect the cancer early,” she said.
Yet, even at that early stage, the treatment involved a major hysterectomy surgery that removed the entire womb, she added.
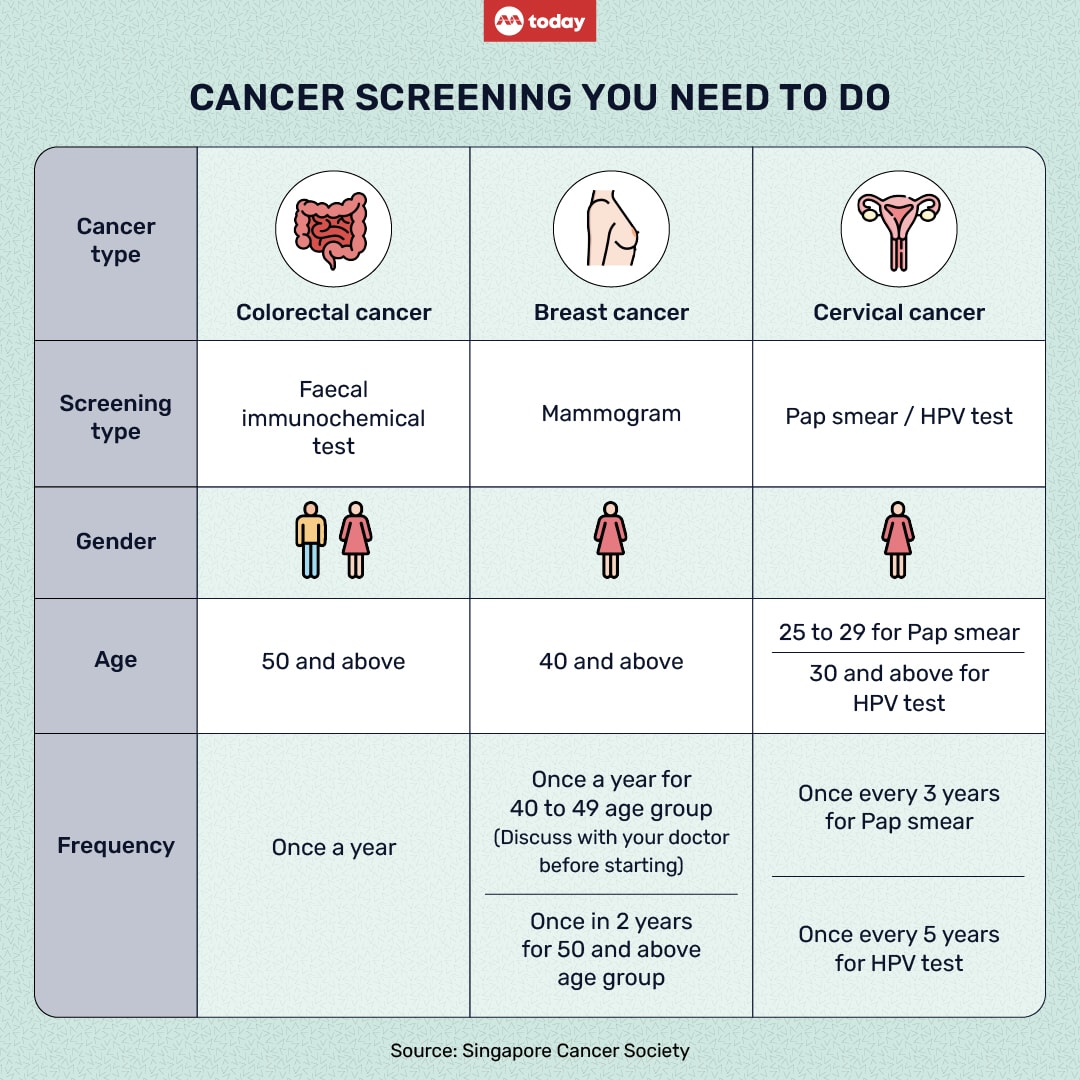
WHAT ARE THE RECOMMENDED CANCER SCREENINGS
Cancer screening may help detect early signs of cancer, sometimes even before symptoms appear.
The Screen for Life programme is a national screening programme that offers eligible Singapore citizens and permanent residents subsidised screenings.
1. For colorectal cancer screening, the faecal immunochemical test — where a small stool sample is collected for a test — is recommended for people aged 50 and above, to be done every year
2. For breast cancer, a mammogram is recommended once every two years for women aged 50 and above. Women in the 40 to 49 age group are also eligible for a mammogram once a year if their doctor has recommended them to go for it
3. For cervical cancer, a Pap smear every three years is recommended for women in the 25 to 29 age group who have ever been sexually active. For those aged 30 and above, a human papillomavirus (HPV) test is recommended every five years.
WHY THE FOCUS ON SCREENING FOR COLON, BREAST AND ‘COMMON’ CANCERS
The screening methods above for colon, breasts and cervix have been shown to effectively detect cancer at an earlier stage.
In some cases, screening may be able to detect even a pre-cancer development, which is the presence of abnormal cells that could pose a greater risk of becoming cancerous.
Colorectal cancer is an example of a well-studied cancer that can be detected even before the actual disease develops.
The faecal immunochemical test is a preliminary cancer screening test that detects the presence of small amounts of blood in stools.
However, the presence of blood does not mean that the person has cancer; further tests are needed.
Dr Melvin Look, a specialist in gastrointestinal cancer surgery and director of PanAsiaSurgery clinic, said that a positive faecal immunochemical test should be followed by colonoscopy for screening.
The procedure for a colonoscopy involves preparation the day before of drinking a laxative solution to clear out all solid contents in the intestines.
Then, for the scope, a long flexible tube with a light and tiny camera is placed through the anus into the end of the large intestine to look for abnormalities along the intestinal walls and tract.
Dr Samuel Ow, Singapore Cancer Society’s council member and chairperson of the society’s community health committee, explained how colonoscopy can potentially detect the cancer at a very early stage, even in a pre-cancer stage.
“We know that there’s a continuum.
“It begins from normal colon tissue, to a benign polyp (benign lumps that form on the inner wall of the colon and rectum), to a polyp that is starting to develop changes, to a pre-cancer polyp, then to invasive cancer.
“This whole developmental process can take a decade or longer.
“Therefore when I speak to my patients about screening for colon cancer, I will pitch to them that I'm actually not trying to detect cancer; I'm trying to detect the precursor of cancer and nip it in the bud.”
Dr Ow is a senior consultant with the department of haematology-oncology at National University Cancer Institute, Singapore.
Dr Look said that the availability and uptake of screening tests in Singapore have helped detect some cancers earlier.
For example, about 42 per cent of men with colorectal cancer are diagnosed in the early stages, compared to 19 per cent for lung cancer.
For women, more than three quarters of them (77 per cent) with breast cancer are diagnosed early, whereas only 37 per cent of stomach cancer is diagnosed in the early stage, he said.
WHY ROUTINE OR FREQUENT SCREENING IS NOT ENCOURAGED FOR OTHER CANCERS
One question you might ask is that why are other forms of “common” cancer such as stomach cancer and lung cancer not on the national screening programme?
And with so many types of cancers to watch for, why are there not more routine screening methods to check every organ?
Dr Tanujaa Rajasekaran, senior consultant medical oncologist at Parkway Cancer Centre, said that not all cancers have well-established screening methods.
Breast, colon and cervical cancers are included in the national screening programmes because they meet several criteria:
• They are relatively common
• There are effective screening methods available
• Early detection has been shown to significantly improve outcomes for these cancers
“On the other hand, even though lung, prostate and stomach cancers are also common, there may be challenges with implementing effective screening programmes for these cancers,” Dr Tanujaa said.
“For example, there may not be highly accurate and cost-effective screening tests available for these cancers that can reliably detect them at early stages.
“Additionally, the risk factors for these cancers may not be as well-understood or easily identifiable as those for breast cancer, colon and cervical cancers.”
Certain screening procedures may also be invasive and pose potential risks that do not justify the benefits of screening an entire population.
For example, the current methods to assess the pancreas is through “very invasive” scopes or computed tomography (CT) scans, which comes with radiation, Dr Ow said.
In Singapore, pancreatic cancer is the 10th most common cancer among men and ninth most common one among women.
However, its aggressive nature makes it the fourth most common cause of cancer deaths here.
Dr Ow said: “You can argue that a colonoscopy (that screens for colon cancer) is very invasive, but the frequency that we do a colonoscopy is typically about every 10 years. And so, that's sort of worth it because we know the continuum is long.
“But for an organ like the pancreas, we don't know what the continuum is. Do we offer this yearly? Can we offer this half yearly?
“Also, how do we get tissues from the pancreas? We will have to do a biopsy through a scope. You can imagine that there's this invasiveness, potential harm, side effects and so forth.”
Dr Ow also said that apart from the potential medical risks, unnecessary invasive screening procedures can affect people psychologically and can be cost- and time-consuming.
There is also now evidence to suggest that screening may sometimes detect cancers that are very slow-growing, or indolent, that may not actually require any treatment, Dr Tanujaa said.
For some slow-growing cancers, the treatment strategy may be just watchful waiting, which means to closely monitor the patient without giving any treatment until changes occur, Dr Ow said.
“Studies have shown that if you do autopsies of elderly men, many of them may have had prostate cancer but they (did not) die of it.
“So that's why there's something called ‘a lead-time bias’, because we don't know whether or not some cancers picked up by tests can affect lifespan or affect quality of life. Prostate cancer that is slow-growing is (an example),” he explained.
Lead-time bias occurs when screening finds a cancer earlier, but the earlier diagnosis does not change the course of the disease.
WHEN TO SCREEN EARLIER FOR CERTAIN CANCER TYPES
The current national screening recommendations for cervical, breast and colon cancer apply to people with average risks and no symptoms.
For those with more risk factors, extra or early screening may be appropriate.
“Individuals with a strong family history of certain cancers may benefit from starting cancer screening at an earlier age or undergoing more frequent screening than the general population,” Dr Tanujaa said, adding that the decision should be made in consultation with a healthcare provider.
For instance, women with a family history of breast cancer, especially if it involves first-degree relatives such as a mother or sister, may be advised to start mammography screening at an earlier age than the general population.
Dr Tanujaa said that it is generally recommended to start breast cancer screening 10 years younger than the first-degree relative was when she was diagnosed with breast cancer.
Genetic counselling and testing for mutations in the BRCA1 and BRCA2 genes may be recommended for those with a strong family history of breast or ovarian cancer, she advised.

People with a family history of colorectal cancer or certain hereditary syndromes, such as Lynch syndrome or familial adenomatous polyposis, may also need to begin colorectal cancer screening earlier than the recommended age of 50.
This may involve starting colonoscopy screening in their 40s or even earlier, depending their family history and genetic testing results, Dr Tanujaa said.
Another example is liver cancer screening for people with a history of liver cirrhosis or chronic hepatitis B infection.
HOW HELPFUL ARE TUMOUR-MARKER TESTS?
Some screening packages include a panel of tumour-marker tests that claim to be able to detect certain cancers early.
However, relying on such tests to screen for cancer can potentially do more harm than good.
Dr Tanujaa said that tumour-marker tests measure certain substances in the blood, urine or tissue that can be elevated in the presence of cancer.
“While they can be useful in some specific situations such as monitoring the response to cancer treatment or detecting cancer recurrence in individuals already diagnosed with cancer, they are generally not recommended for routine cancer screening in asymptomatic individuals,” she added.
Dr Look from PanAsia Surgery said that due to its low sensitivity, cancer markers are not useful as a cancer screening test.
“Cancer markers can be totally normal even in a patient with a very advanced cancer, and it may give a false sense of security in assuring the patient that he or she doesn’t have cancer.
“Cancer markers can also be elevated due to non-cancer causes, causing a false sense of alarm when they are used for general screening,” he added.
WHAT TO KNOW BEFORE GOING FOR CANCER SCREENING
It helps to understand your personal health history before you put a chunk of money down for screening tests.
“Knowing your family history of cancer, previous cancer diagnoses and other relevant medical conditions can help individuals assess their own risk factors for specific types of cancer,” Dr Tanujaa said.
She also advised people to educate themselves on the recommended screening guidelines, based on age, gender and other risk factors.
They may consult their healthcare providers to get more personalised recommendations.
Dr Ow from the Singapore Cancer Society said that it is also important to follow the recommended screening schedule, or as advised by a doctor.
“(Cancer screening schedules) are not static,” he said.
“For example, for HPV and Pap smears, the schedule may be between every three and five years, but there’s also an adapted strategy.
“If there are some slight changes that need to be followed up on, it may not be three to five years later; it may be six to 12 months."
And just because you go for a screening once under the recommended guidelines and the results are normal, it does not mean that you can stop doing the checks forever and do not keep up the schedule for the next check. It is not a one-time-only thing.
Dr Ow said: “We have patients with abnormal mammogram (findings) who did a biopsy, found out that it’s benign, everything’s normal, and that's the last mammogram they went for (and they do not do it again) because they felt that everything was okay."
For the Screen for Life programme available to Singaporeans and permanent residents, go to its website for more information.
To book a screening with the Singapore Cancer Society, go to its website to find out more.








